Pus cells in CSF: Introduction, Possible Conditions, Laboratory Diagnosis and Treatment
Pus cells in CSF
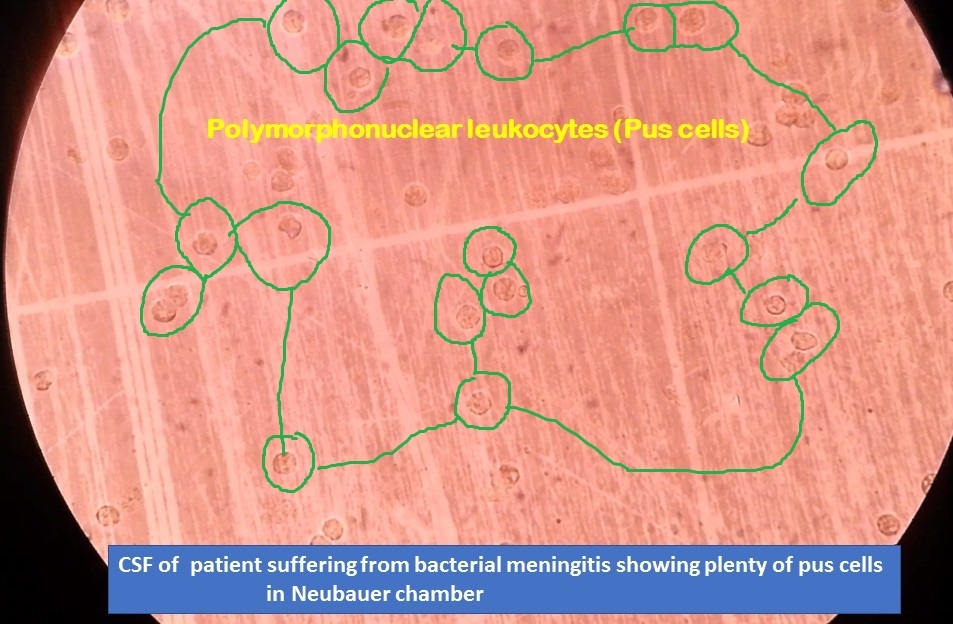
Pus cells( dead leukocytes especially neutrophils) in CSF as shown above image and photo taken during microscopy of CSF charging Improved Neubauer chamber at 40X objective. This condition is an indicator of pyogenic meningitis due to the presence of polymorphonuclear leucocytes (‘pus cells’) in cerebrospinal fluid (CSF). This virtually excludes infection with viruses, rickettsiae, fungi, and, except in the acute stages, with the tubercle bacillus. It is a serious condition even though the mortality and morbidity of this condition have decreased considerably since the introduction of chemotherapy. Pus is a thick fluid containing dead tissue, cells, and bacteria. Our body often produces it when it’s fighting off an infection, especially infections caused by bacteria.
Possible conditions
Types of meningitis are mainly two types-
- Infectious meningitis and
- Non-infectious meningitis
Infectious Meningitis
Infectious ( due to microorganisms) meningitis is further divided into the following categories-
- Viral meningitis: It is due to viruses like coxsackievirus A, coxsackievirus B, echoviruses, West Nile virus, influenza, mumps, HIV, measles, herpes viruses, and Coltivirus, that causes Colorado tick fever.
- Bacterial meningitis: This type of meningitis is due to bacteria such as Streptococcus pneumoniae (pneumococcal meningitis), Neisseria meningitidis (meningococcal meningitis), Haemophilus influenzae
Listeria monocytogenes, Staphylococcus aureus (staphylococcal meningitis), Streptococci, Klebsiella species, Pseudomonas species, E. coli, Proteus species, etc. - Fungal meningitis: The common causative agent of this type of meningitis are Cryptococcus, Blastomyces, Histoplasma, and Coccidioides. Among them, Cryptococcus neoformans is the most common which causes cryptococcal meningitis.
- Parasitic meningitis: Etiological agents of parasitic meningitis are Angiostrongylus cantonensis, Baylisascaris procyonis, Gnathostoma spinigerum, and rarely Naegleria fowleri (amebic meningitis). Parasitic meningitis is also called eosinophilic meningitis (EM).
Non-infectious meningitis
There is no involvement in infection in non-infectious meningitis. Instead, it is a type of meningitis that is caused by other medical conditions or treatments e.g. lupus, a head injury, brain surgery, cancer, and certain medications.
Impression
The presence of plenty of pus cells (neutrophils) in CSF is an indicator of pyogenic meningitis. The causative agents of pyogenic meningitis are bacteria ( bacterial meningitis) and rarely parasite, Naegleria fowleri (parasitic meningitis, amebic meningitis).
What do the levels of pus cells in specimens indicate?
In the case of urine, normal numbers of pus cells are up to 5 in males and may be up to 10 in females at high per field (HPF). The presence of pus cells in urine is also called pyuria and is defined as >10 pus cells per microlitre (µl) of urine.
Whereas in the case of CSF, a single pus cell is significant to be an infection.
Sign and symptoms of meningitis
Sign
- Fever
- Headache
- Vomiting
- Irritability
- Fits
- Photophobia
- Earache
Symptoms
- Neck rigidity
- Kernig’s
- Alteration in consciousness
- Petechiae
- Papilloedema
- Ocular palsy
- Hemiparesis
- Tetraparesis
- Tense fontanelle
- Opisthotonos
Causative organisms of pyogenic meningitis
- Meningococcus (Neisseria meningitidis )
- Haemophilus influenzae type B
- Pneumococcus (Streptococcus pneumoniae)
- Listeria monocytogenes
- Streptococci
- Staphylococci
- Klebsiella species
- Pseudomonas species
- E. coli
- Proteus species
- Naegleria fowleri ( rare case)
Laboratory Diagnosis
CBC Count: A complete blood count with differential is a general index of health. It checks the number of red blood cells, platelets, and white blood cells in our blood. White blood cells ( leukocytes) fight infection. The count is usually elevated in meningitis.
Blood cultures: To identify bacteria in the blood. Bacteria can travel from the blood to the brain. Neisseria meningitidis and Streptococcus pneumoniae, among others, can cause both sepsis and meningitis.
Imagine: Computerized tomography (CT) or magnetic resonance imaging (MRI) scans, X-rays
Spinal tap (lumbar puncture): For a definitive diagnosis of meningitis, there is a need for a spinal tap to collect cerebrospinal fluid (CSF). In people with meningitis, the CSF often shows a low glucose level along with an increased leukocytes count and increased protein.
CSF analysis:
- CSF wet mount
- CSF Gram stain
- CSF India ink preparation
- CSF culture and sensitivity
- CSF DNA based test is known as PCR
- CSF antibodies detection: A test to check for antibodies against certain viruses to determine the specific cause and determine the proper treatment.
Treatment of Meningitis
Treatment depends on the involvement of causative agents of meningitis like bacterial meningitis which requires immediate hospitalization. Early diagnosis and treatment, no doubt, will prevent brain damage and death. It is treated with intravenous antibiotics and selective antibiotics depends on the bacteria involved. Similarly, fungal meningitis is treated with anti-fungal drugs. Parasitic meningitis may either involve treating just the symptoms or attempting to treat the infection directly. Depending on the cause, this type may get better without using anti-parasitic drugs. If it worsens, however, the clinician may try to treat the infection itself. Now about viral meningitis, it may resolve on its own, but some causes of viral meningitis will be treated with intravenous antiviral treatment.
Keynotes
- Bacterial meningitis is still to be a major cause of morbidity and mortality with infants most susceptible. The causative organisms remain largely unchanged but the antibiotics sensitivity pattern revealed increasing resistance to commonly used antimicrobial agents. Multiple seizures, neck retraction, and coma at presentation as well as hyponatremia, hyperglycemia, and turbid CSF increase the risk of death in childhood due to bacterial meningitis.
- Are pus cells in CSF always associated with only bacterial meningitis? The answer is no because in a case amebic meningoencephalitis ( Naegleria fowleri, a free-living thermophilic amoeba found in warm freshwater, enters the nose and migrates to the brain) similar finding with plenty of pus cells in CSF, can misguide the microbiologist as well as the physician. With the passing of time, antimicrobial patients will rapidly deteriorate. So, in every pyogenic meningitis, wet film preparation must be done to exclude primary meningoencephalitis by seeing the motile amoeba, particularly in the case of elderly patients.
Bibliography
- https://www.healthline.com/health/pus
- https://pmj.bmj.com/content/postgradmedj/43/499/376.full.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4692015/
- https://anesthesiology.pubs.asahq.org/article.aspx?articleid=1934439
- https://doctor.ndtv.com/faq/what-do-the-levels-of-pus-cells-in-urine-indicate-11172
- https://www.researchgate.net/post/Are_pus_cells_in_CSF_always_associated_with_only_bacterial_meningitis
- https://www.healthgrades.com/right-care/symptoms-and-conditions/pus
- https://www.medicalnewstoday.com/articles/249182
- https://en.wikipedia.org/wiki/Pus
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2018983/pdf/archdisch01591-0064.pdf
- http://www.journalofdiabetology.org/article.asp?issn=2078-7685;year=2019;volume=10;issue=3;spage=102;epage=109;aulast=Patra
- https://www.kidney.org/atoz/content/what-urinalysishttps://advuro.com/urinary-conditions/pyuria/
- https://adc.bmj.com/content/archdischild/44/236/480.full.pdf
- https://www.verywellhealth.com/what-is-pyuria-3522705
