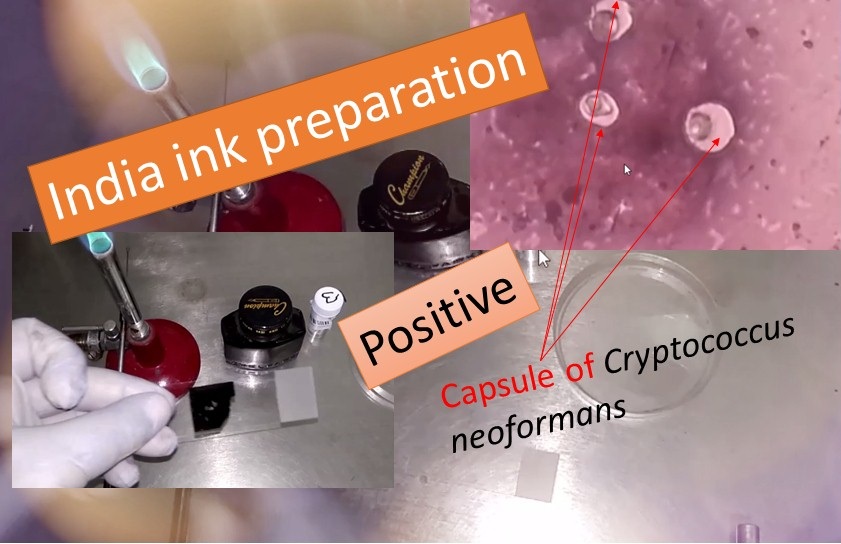
India Ink Preparation when Cryptococcal meningitis is suspected
Introduction
Cryptococcal meningitis occurs in immunodeficient patients and when meningitis is clinically suspected, for example, patients with HIV disease, or when yeast cells with lymphocyte are detected when performing C.S.F. cell count or examine Gram smear, examine India ink preparation for encapsulated yeasts. India ink is used as a negative stain in negative staining that uses ion negative staining method permits visualization of the usually transparent and unstainable capsules of various micro- microorganisms like Cryptococcus neoformans (most commonly), Klebsiella pneumoniae, Streptococcus pneumoniae, etc.
Principle of India Ink
The capsule is non-ionic so that the India ink used will not bind to it. This is the reason, capsule appears as a clear halo around the yeast cells.
Composition of India Ink
( Hardy Diagnostics)
- Black Pelican Drawing Ink No. 17
- Deionized Water
- Thimerosal
Requirements for India Ink Preparation
- India ink or nigrosin stain
- Clean and grease-free slide and coverslips
- C.S.F. specimen
- Droppers or inoculating loop
- Waste discarding container or Bunsen burner
- Centrifuge
- Test tubes
- Microscope
- Control stains ( For positive control Cryptococcus neoformans
ATCC® 32045 while for negative control Candida albicans ATCC® 10231)
Procedure of India Ink Preparation
- Centrifuge the CSF for 5 to 10 minutes.
- Remove the supernatant fluid and mix the sediment.
- Transfer an equal amount of sediment and India ink i.e. a drop of the sediment to a slide and add a drop of India ink.
- Mix and cover with a coverslip.
- Now, examine the preparation under a microscope using the 40 X objective.
Observation of India Ink Preparation
Look for oval or round cells, some showing budding, irregular in size, measuring 2-10 µm in diameter, and surrounded by a large unstained capsule as shown in the above figure. Very rarely capsules are absent.
Result Interpretation
- Encapsulated yeasts are seen: Positive
- Non-encapsulated yeast cells: Negative
- Positive control: Presence of encapsulated yeasts seen
- Negative control: Absence of encapsulated yeasts seen
- Test: Positive as shown above image.
Report
Capsules of Cryptococcus neoformans like organisms seen
Importance of this test
When encapsulated yeasts are detected in C.S.F. a presumptive diagnosis of cryptococcal meningitis can be made.
Key Notes
- Pelikan black drawing ink is suitable for this test.
- When India ink is not available, use the nigrosin (20% w/v) solution.
- Do not make the preparation too thick otherwise, the cells and capsules will not be seen.
Limitations of Ink Ink or Negative staining
- India ink preparation is only for presumptive identifications of organisms and therefore it needs other tests like biochemical, immunological, molecular, or mass spectrometry testing that must be performed on colonies from pure culture for complete identification.
- Fat droplets, white blood cells, and tissue cells are sometimes confused with organisms like Cryptococcus neoformans cells. Leukocytes and tissue cells may be dissolved by adding a drop of 10% KOH.
- Some strains of Cryptococcus neoformans , as well as other cryptococci, may not produce discernible capsules in vitro.
Other Information related to Cryptococcus
Cryptococcus capsule in Giemsa stained smear as shown below-
Cryptococcus neoformans growth on Sabouraud Dextrose Agar (SDA) Bird Seed Agar (BSA)- Niger seed is replaced by Nescafe Coffee and Urea Hydrolization Test-Positive as shown in Video-
Cryptococcus neoformans in LPCB tease mount as shown below-
Further Readings
- Medical Mycology. Editors: Emmons and Binford, 2nd ed 1970, Publisher Lea and Febiger, Philadelphia.
- Rippon’s JW: Medical Microbiology. The pathogenic fungi and the Pathogenic Actinomycetes. 3rd ed 1988 Publisher WB Saunder co, Philadelphia.
- Clinical Microbiology Procedure Handbook Vol. I & II, Chief in editor H.D. Isenberg, Albert Einstein College of Medicine, New York, Publisher ASM (American Society for Microbiology), Washington DC.
- A Text-Book of Medical Mycology. Editor: Jagdish Chander. Publication Mehata, India.
- Practical Laboratory Mycology. Editors: Koneman E.W. and G.D. Roberts, 3rd ed 1985, Publisher Williams and Wilkins, Baltimore.
- Topley & Wilsons Medical Mycology. Editors: M.T. Parker & L.H. Collier, 8th ed 1990, Publisher Edward Arnold publication, London.
- Textbook of Diagnostic Microbiology. Editors: Connie R. Mahon, Donald G. Lehman & George Manuselis, 3rd edition2007, Publisher Elsevier.
- Mackie and Mc Cartney Practical Medical Microbiology. Editors: J.G. Colle, A.G. Fraser, B.P. Marmion, A. Simmous, 4th ed, Publisher Churchill Living Stone, New York, Melborne, Sans Franscisco 1996.
- http://himedialabs.com/TD/S025.pdf
- Bailey & Scott’s Diagnostic Microbiology. Editors: Bettey A. Forbes, Daniel F. Sahm & Alice S. Weissfeld, 12th ed 2007, Publisher Elsevier.
- https://www.sciencedirect.com/topics/medicine-and-dentistry/indian-ink
- https://en.wikipedia.org/wiki/Cryptococcus_neoformans
- https://catalog.hardydiagnostics.com/cp_prod/content/hugo/indiaink.htm
