Blood agar showing beta hemolytic colony: Introduction, Possible organism and its details
Introduction
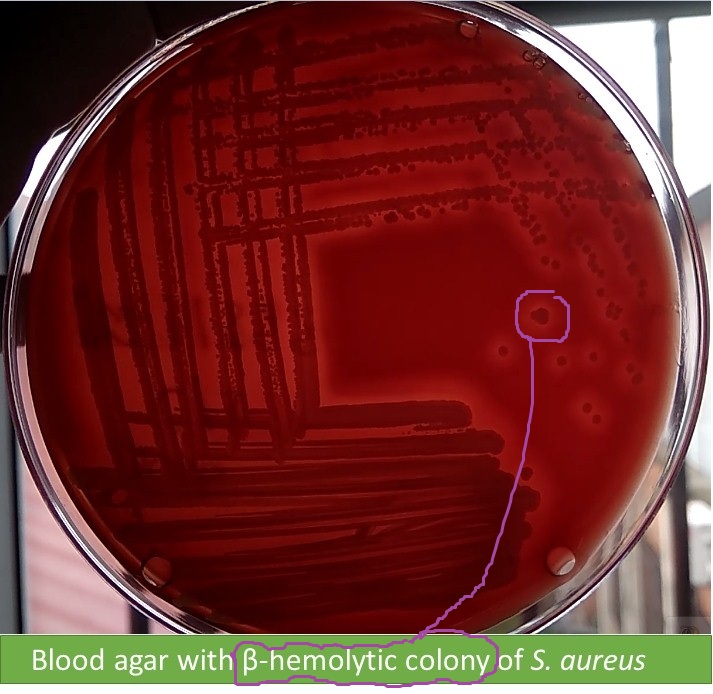
5% sheep blood agar is with beta (β) hemolytic colony of Staphylococcus aureus as shown above image. Colonies of Streptococcus agalactiae , Streptococcus pyogenes are also beta hemolytic on blood agar but they are pin point where as S. aureus pin head and catalase test positive. Streptococci are catalase test negative.
Staphylococcus aureus
Definition
Spherical, non motile, gram positive, cluster forming. On nutrient agar , growth is opaque and golden yellow or white color. Catalase test positive, coagulase test positive, oxidase negative , aerobic or facultative anaerobe. Parasite of human and animal.
Habitat
Normal flora of skin, upper respiratory tract and feces of human, animal and birds too.
Morphology
- Round or spherical arranged in clusters.
- 0.8-1.0 μm in size
- Non motile, non sporing, usually non encapsulate while some strains are encapsulate. Capsule is of two types
- Micro capsule <200 nm
- Macro capsule >200 nm and is responsible for slime layer
Cultural characteristics
On nutrient agar
- Smooth, circular, often yellow pigmented colonies and non diffusible.
- 1-2 mm in diameter
- Butyrous in consistency
On blood agar
Pigmentation
Golden yellow and increased in the presence of CO2 and also at room temperature. Pigmentation can be induced by culturing bacteria into 30% milk agar, potato and 1% glycerol monoacetate or phosphate agar.
Selective media for Staphylococcus
- 7-10% salt agar
- Mannitol salt agar
- Tellurite glycine agar
- Phenolphthalien phosphate agar
- Polymyxin B agar (75 μg/ml)
Note: Staphylococcus aureus grow well on this medium but coagulase negative Staphylococci (CoNS) can not grow.
Resistance
Thermal death point of Staphylococcus aureus is 60°C for 30 minutes.
It can survive in dried pus for 2-3 months.
Cell wall
Protein -A: It has specific affinity for Fc portion of the IgG molecule (except Ig3) leaving the Fab region free to combine with its specific antigen resulting in agglutination known as coagglutination. Peptidoglycan of cell activates complement and induces release of inflammatory cytokines. Similarly teichoic acid of cell wall facilitates adhesion of the cocci to the host cell surface.
Phage types
With the use of 28 phages, several hundred phage types have been identified among them important phage types are-
- Group 1: 8052A/79 (Hospital strains)
- Group 2: 3B/3C/55 (Impetigo / Staphyococcal Scalded Syndrome)
- Group 3: 6/47 (Enterotoxin producer)
Serotype
There are 30 serotypes based on protein A antigen.
Enzyme and toxins
Toxins
- Haemolysin: alpha, beta, gamma
- Leucodin
- Enterotoxin A-F
- Type A and B are responsible for food poisoning.
- 25 µg of toxin B can cause food poisoning.
- Epidermolytic toxin: It is responsible for Staphylococcal Scalded Syndrome (SSS) or Ritter’s disease.
- Toxic Shock Syndrome Toxin (TSST): Type -F
Enzymes
Coagulase : It is of two types bound and free coagulase.
Phosphatase
Staphylokinase
Hyluronidase
Lipase
Prptease
Pathogenecity of Staphylococcus aureus
Staphylococcus aureus can cause following diseases-
- Abscess
- Conjunctivitis
- Corneal ulcer
- Septicemia
- Endocarditis
- Pneumonia
- Mastitis: It is an inflammation of breast.
- Empyemia : It is accumulation of pus in the body cavity.
- Food poisoning
- Staphylococcal Scalded Syndrome
- Toxic Shock Syndrome (TSS)-enterotoxin F
- Septic arthritis
- Meningitis
- Osteomyelitis
Laboratory Diagnosis of Staphylococcus aureus
Samples/ specimens collection
It depends on according to site of infection and the nature of lesion. e.g.
Pus (Suppurative lesion)
CSF ( meningitis)
Blood (septicemia)
Sputum( respiratory infection)
Nasal swab (detection of carriers)
Feces and remains of food (food poisoning)
Gram stain: Gram positive cocci in cluster
Culture
Media -for routine Nutrient agar and blood agar
for Selective
- 7-10% salt agar
- Mannitol salt agar
- Tellurite glycine agar
- Phenolphthalien phosphate agar
- Polymyxin B agar (75 μg/ml)
Colony characteristics
on nutrient agar
Smooth, circular, often yellow pigmented colonies and non diffusible.
-1-2 mm in diameter
Butyrous in consistency
On blood agar
Beta haemolytic
Biochemical tests
Catalse test: Positive
Oxidation and fermentation (OF) test: Fermentative
Coagulase test: Positive
DNAse test : Positive
From these features organism is identified as Staphylococcus aureus.
Coagulase test
Coagulase brings about the clotting of plasma which is similar to thrombin -catalytic conversion of fibrinogen into fibrin.
Types
- Free coagulse : This is an extracelluar enzyme of bacteria secreted into the medium. It is thrombin like substance which can nealy fibrinogen to fibrin. Tube coagulase test is performedn for its detection.
- Bound coagulase: This is closely bound to the cell wall . On its surface , it has receptors for fibrinogen so that fibrin forms link between the bacteria. This cause the clumping of Staphylococci. Hence , bound coagulase is also known as clumping factor. Slide coagulate test is done for its detection.
Treatment
Following antibiotics are available for antibiotics sensitivity test (AST)-
- Clindamycin
- Erythromycin
- Cefoxitin
- Chloramphenicol
- Ciprofloxacin
- Gentamycin
- Ofloxacin
- Cotrimoxazole
- Doxycycline
- Vancomycin
- Teicoplanin
- Linezolid
- Nitrofurantoin
Key Notes
- Nitrofurantoin is only applicable in case of urinary tract infection replacing chloramphenicol.
- To treat Methicillin-resistant Staphylococcus aureus (MRSA), vancomycin is recommended where as to treat Vancomycin-resistant Staphylococcus aureus (VRSA), linezolid is preferred.
References
- Bailey & Scott’s Diagnostic Microbiology. Editors: Bettey A. Forbes, Daniel F. Sahm & Alice S. Weissfeld, 12th ed 2007, Publisher Elsevier.
- Clinical Microbiology Procedure Hand book, Chief in editor H.D. Isenberg, Albert Einstein College of Medicine, New York, Publisher ASM (American Society for Microbiology), Washington DC.
- Colour Atlas and Text book of Diagnostic Microbiology. Editors: Koneman E.W., Allen D.D., Dowell V.R. Jr and Sommers H.M.
- Jawetz, Melnick and Adelberg’s Medical Microbiology. Editors: Geo. F. Brook, Janet S. Butel & Stephen A. Morse, 21st ed 1998, Publisher Appleton & Lance, Co Stamford Connecticut.
- Mackie and Mc Cartney Practical Medical Microbiology. Editors: J.G. Colle, A.G. Fraser, B.P. Marmion, A. Simmous, 4th ed, Publisher Churchill Living Stone, New York, Melborne, Sans Franscisco 1996.
- Manual of Clinical Microbiology. Editors: P.R. Murray, E. J. Baron, M. A. Pfaller, F. C. Tenover and R. H. Yolken, 7th ed 2005, Publisher ASM, USA
- Text book of Diagnostic Microbiology. Editors: Connie R. Mahon, Donald G. Lehman & George Manuselis, 3rd edition2007, Publisher Elsevier.
- Topley & Wilsons Principle of Bacteriology, Virology and immunology. Editors: M.T. Parker & L.H. Collier, 8th ed 1990, Publisher Edward Arnold publication, London.
- District Laboratory Practice in Tropical Countries – Part-2- Monica Cheesebrough- 2nd Edn Update
