Fungal UTI: Introduction, Sign and Symptoms, Complication, Lab Diagnosis and Treatment
Introduction of Fungal UTI
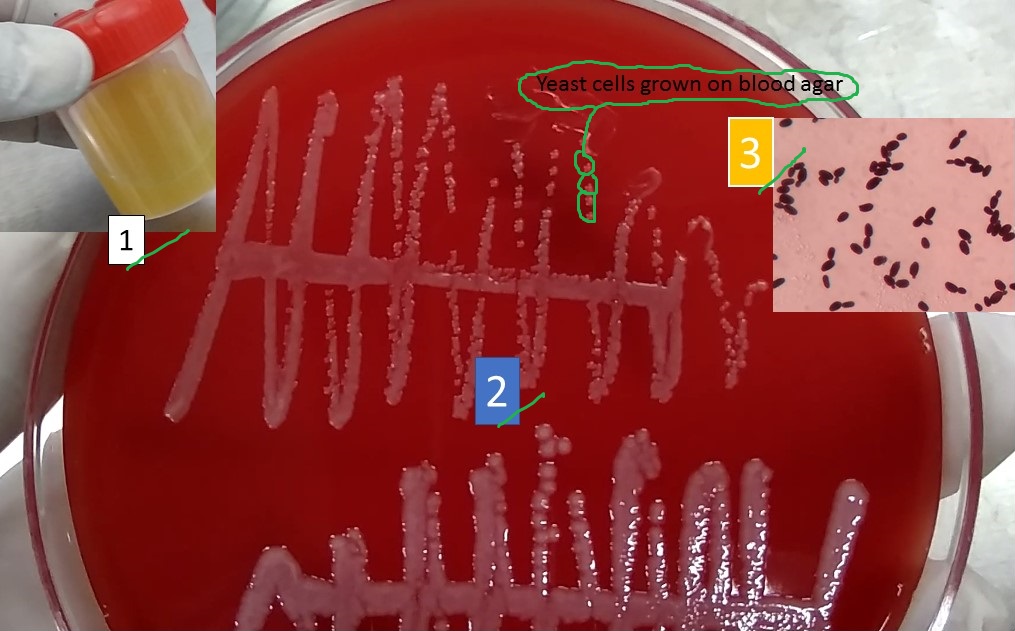
Urinary tract infection (UTI) is due to Candida as shown above picture. Fungal UTI is due to Candida is most common and it is the normal commensals in humans. Its colonization differs from infection in which infection produces tissue reaction. All invasive fungi like Cryptococcus neoformans, Aspergillus , Mucoraceae , Histoplasma capsulatum, Blastomyces , Coccidioides immitis may infect the kidneys as part of a systemic or disseminated mycotic infection. Among them alone responsible for infection.
Lower UTI with Candida usually occurs in patients with urinary catheters, typically after antibiotic therapy, even though candidal and bacterial infections frequently occur simultaneously. prostatitis due to Candida albicans occurs infrequently in patients with diabetes, usually after instrumentation.
Renal candidiasis normally occurs gastrointestinal tract origin hematogenous spread. Ascending infection is possible and happens mainly in patients with nephrostomy tubes, other permanent indwelling devices, and stents. At high risk are patients with diabetes and also those who are immunocompromised because of tumors, AIDS, chemotherapy, or immunosuppressants. A major source of candidemia in such high-risk hospitalized patients is an indwelling intravascular catheter. Renal transplantation is also responsible to increase the risk because of the combination of indwelling catheters, stents, antibiotics, anastomotic leaks, obstruction, and immunosuppressive therapy.
Sign and Symptom of Fungal UTI
Normally patients with candiduria are asymptomatic but Candida can cause urethral symptoms like mild urethral itching, dysuria, watery discharge in females may result from the urine coming into contact with periurethral tissue that is inflamed due to candidal vaginitis. Among lower UTI, cystitis due to Candida may result in frequency, urgency, dysuria, and suprapubic pain. Hematuria is common. In patients with poorly controlled diabetes, pneumaturia due to emphysematous cystitis has occurred. Fungus balls may cause symptoms of urethral obstruction. Most patients with renal candidiasis that is hematogenously spread lack symptoms referable to the kidneys but may have an antibiotic-resistant fever, candiduria, and unexplained deteriorating renal function.
Complications of Fungal UTI
Complications of fungal UTI due to candidal infection can include emphysematous cystitis or pyelonephritis and fungus balls in the renal pelvis, ureter, or bladder. Lower or upper urinary tract obstruction may occur. Papillary necrosis and intrarenal and perinephric abscesses may form. Although renal function often declines, severe renal failure is rare without postrenal obstruction.
Lab Diagnosis of Fungal UTI
Urine R/E and culture
Urethral discharge culture
Treatment of Fungal UTI
Treatment of fungal UTI fully depends on nature and severity of infection for symptomatic or high-risk patients fluconazole or, for resistant organisms, amphotericin B; sometimes flucytosine is added. Fungal colonization of catheters does not require treatment. Asymptomatic candiduria rarely requires therapy. Candiduria should be treated in the following:
- Neutropenic patients
- Symptomatic patients
- Patients who are undergoing urologic manipulation
- Patients with renal allografts
Further Readings
- Medical Mycology. Editors: Emmons and Binford, 2nd ed 1970, Publisher Lea and Febiger, Philadelphia.
- Rippon’s JW: Medical Microbiology. The pathogenic fungi and the Pathogenic Actinomycetes. 3rd ed 1988 Publisher WB Saunder co, Philadelphia.
- Clinical Microbiology Procedure Handbook Vol. I & II, Chief in editor H.D. Isenberg, Albert Einstein College of Medicine, New York, Publisher ASM (American Society for Microbiology), Washington DC.
- A Textbook of Medical Mycology. Editor: Jagdish Chander. Publication Mehata, India.
- Practical Laboratory Mycology. Editors: Koneman E.W. and G.D. Roberts, 3rd ed 1985, Publisher Williams and Wilkins, Baltimore.
- Textbook of Diagnostic Microbiology. Editors: Connie R. Mahon, Donald G. Lehman & George Manuselis, 3rd edition2007, Publisher Elsevier.
- Mackie and Mc Cartney Practical Medical Microbiology. Editors: J.G. Colle, A.G. Fraser, B.P. Marmion, A. Simmous, 4th ed, Publisher Churchill Living Stone, New York, Melborne, Sans Francisco 1996.
- https://www.msdmanuals.com/professional/genitourinary-disorders/urinary-tract-infections-utis/fungal-urinary-tract-infections
- Bailey & Scott’s Diagnostic Microbiology. Editors: Bettey A. Forbes, Daniel F. Sahm & Alice S. Weissfeld, 12th ed 2007, Publisher Elsevier.
