Malassezia: Introduction, Classification, Pathogenecity, Laboratory Diagnosis and Treatment
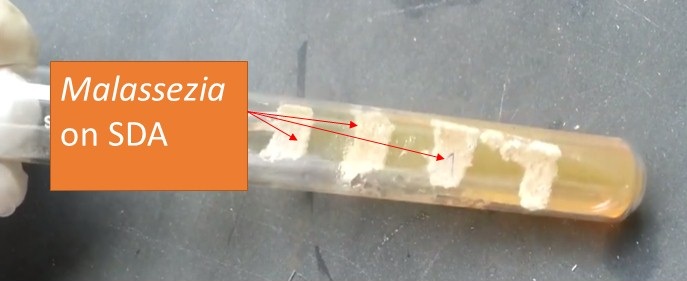
Malassezia on SDA
Malassezia growth on SDA as shown above picture. Malassezia is a monophyletic genus of fungi known to man for more than 150 years as a commensal and pathogen. French scientist Louis-Charles Malassez identified Malassezia in the late 19th century. Raymond Sabouraud identified a dandruff-causing organism in 1904 and called it “Pityrosporum malasseez”, honoring Malassez. They are a ubiquitous component of the human skin microbiome and are associated with a myriad of skin problems, including dandruff in billions of people and rarely found in places other than on skin. 7 billion people are involved with a variety of conditions, including dandruff, atopic eczema (AE) /dermatitis, pityriasis versicolor, seborrheic dermatitis (SD), and folliculitis. In immunocompromised hosts they can also cause systemic infections.
Taxonomic Classification
(described by Baillon in 1889)
- Kingdom: Fungi
- Phylum: Basidiomycota
- Class: Hymenomycetes
- Order: Tremellales
- Family: Filobasidiaceae
- Genus: Malassezia
- Genus Malassezia comprises 14 species of “yeast-like fungi,” 13 of which are lipophilic and 1 is nonlipophilic( M. pachydermatis) and they are-
- M. furfur,
- M. pachydermatis,
- M. sympodialis,
- M. globosa,
- M. obtusa
- M. restricta,
- M. slooffiae,
- M. equina,
- M. dermatis,
- M. japonica,
- M. nana,
- M. capre,
- M. yamatoensis, and most recently
- M. cuniculi.
Pathogenicity
Malassezia can cause both localized ( common) i.e. superficial mycoses and systemic ( rare) infections. Skin involved Malassezia infections are-
- Pityriasis versicolor – It is most often due to the subspecies Malassezia globosa, M. sympodialis, and M. furfur.
- Malassezia folliculitis is due to the yeast growing in the hair follicles where they produce inflammation and risk factors for this infection are immunosuppression, diabetes mellitus broad-spectrum antibiotics, use of steroids, puberty, pregnancy, and application of cosmetics, lotions, sunscreens, emollients, olive oil which cause occlusion of the skin.
- Steroid acne
- Seborrhoeic dermatitis, dandruff, sebopsoriasis, and facial or scalp psoriasis are the most often due to M. restricta and M. globosa.
- Neonatal cephalic pustulosis (neonatal acne), a pustular eruption on young babies that resembles infantile acne.
- Cradle cap: Infantile or neonatal SD is also known as pityriasis capitis, crusta lactea, milk crust, non-itching lesion on the scalp of newborn.
- Possibly, some cases of confluent and reticulated papillomatosis, are a pigmented eruption occurring mainly on the chest, back, and neck of adolescent girls.
- Some facial atopic dermatitis: In this case, there may be specific immunoglobulin E ( IgE) antibodies directed against Malassezia and positive prick tests to the organism.
- Rarely, invasive pityrosporosis occurs in immunodeficient individuals.
Factors responsible for overgrowth of Malassezia in our body
Geographical: Geographical variations are responsible for the densities of different Malassezia species on the skin. It is seen more commonly in the warm and humid tropical and subtropical climates which is more suited for its growth. e.g. Malassezia globosa tends to increase in summer when temperatures are high and due to sweat.
Age: Pityriasis versicolor (PV) is common 20 to 40 years of age but in India, the age group is between 10 and 30 years.
Hormonal factors: Patients who are on corticosteroid therapy, malnutrition, and increased plasma cortisol levels have been shown to mediate pityriasis versicolor.
Pathogenesis: Human sebum is the lipid source where these yeasts enjoy because it is a complex mixture of lipids. Thus, alteration in sebum secretion and its breakdown helps in the development of dandruff. Malassezia infections are also associated with hyperhidrosis.
Laboratory Diagnosis
Specimen: skin scrapings
Direct Microscopy: Potassium hydroxide (KOH) preparations of skin scrapings shows clusters of yeast cells having the shape of globose, oblong -ellipsoidal, and short hyphae.
Fungal culture: Inoculation of specimens on SDA containing cycloheximide ( actidione) with olive oil or Dixon’s agar which contains glycerol mono-oleate. Colonies are cream to yellowish, smooth or slightly wrinkled, glistening or dull, and with the margin being entire or lobate.
LPCB preparation from culture: It shows globose, oblong -ellipsoidal yeast cells, and short hyphae.
Histological examination: Yeasts may also be detected within the stratum corneum on histopathology of a skin biopsy; they are best seen using special stains such as periodic acid-Schiff (PAS).
Molecular Identification: Sequencing of ITS and D1/D2 regions of rDNA can be used for molecular identification.
Treatment
The anti-fungal mechanism of action has recently been described for one commonly used anti-dandruff shampoo active ingredient, zinc pyrithione (ZPT). Based on the ionophore properties of pyrithione and the demonstrated increase in mammalian cell zinc levels upon ZPT treatment, it was expected that ZPT would act by delivering high intracellular zinc levels to inhibit fungal growth. In general, Malassezia infections are treated with topical or oral antifungal agents, such as ketoconazole shampoo and oral fluconazole. Seborrhoeic dermatitis may also be treated with topical steroids.
Keynotes
- Among the Basidiomycota, only Malassezia and Cryptococcus are frequent human pathogens.
- Earlier, the hyphae filaments used to be called ‘Malassezia’, and the yeast forms were called ‘Pityrosporum’, but mycologists eventually realized they were the same organism.
- Catheter-related bloodstream infections (CRBSI) due to Malassezia among newborns receiving total parenteral nutrition (TPN), and in immunocompromised elderly receiving parenteral lipid supplements has also been reported.
- Fungemia and sepsis due to Malassezia furfur and M. pachydermatis may occur particularly in the immunocompromised elderly.
- M. pachydermatis, which is lipophilic but not lipid-dependent.
- Molecular-based methods such as Polymerase Chain Reaction techniques, and Matrix-Assisted Laser Desorption/Ionization—Time Of Flight mass spectrometry, and the chemical imprint method Raman spectroscopy is very useful tools for species identification.
- Molecular Identification: ITS and D1/D2 sequencing may be used for accurate species identification.
- MALDI-TOF MS: Capable of identifying all 14 Malassezia species in concordance with those of ITS sequence analyses.
- Malassezia species are difficult to grow in the laboratory on ordinary mediums lacking natural or olive oil so scrapings may be reported as ‘culture-negative since they grow best if a lipid such as olive oil is added to Littman agar culture medium or SDA.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3380954/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533528/
- https://dermnetnz.org/topics/malassezia-infections/
- https://www.frontiersin.org/articles/10.3389/fcimb.2020.00112/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC540166/
- https://mycology.adelaide.edu.au/descriptions/yeasts/malassezia/
- Medical Mycology. Editors: Emmons and Binford, 2nd ed 1970, Publisher Lea and Febiger, Philadelphia.
- Rippon’s JW: Medical Microbiology. The pathogenic fungi and the pathogenic Actinomycetes. 3rd ed 1988 Publisher WB saunder co, Philadelphia.
- Clinical Microbiology Procedure Hand book Vol. I & II, Chief in editor H.D. Isenberg, Albert Einstein College of Medicine, New York, Publisher ASM (American Society for Microbiology), Washington DC.
- A Text Book of Medical Mycology. Editor: Jagdish Chandar. Publication Mehata, India.
- Practical Laboratory Mycology. Editors: Koneman E.W. and G.D. Roberts, 3rd ed 1985, Publisher Williams and Wilkins, Baltimore.
