Introduction
A Synovial Fluid Culture and Sensitivity Test is a medical diagnostic procedure used to evaluate the presence of infection in a person’s joint, specifically within the synovial fluid that surrounds and lubricates joints. The synovial fluid is a clear, viscous fluid that helps reduce friction in joints and provides nourishment to the cartilage. When an infection or inflammation occurs within a joint, it can lead to conditions such as septic arthritis or other joint disorders.
Here’s an introduction to the Synovial Fluid Culture and Sensitivity Test:
- Purpose: The primary purpose of this test is to identify and diagnose infections within the joint space, determine the causative microorganism (bacteria, fungi, or other pathogens), and assess their sensitivity to specific antibiotics or antimicrobial agents. This information is crucial for guiding appropriate treatment decisions.
- Indications: This test is typically ordered when a patient presents with symptoms of joint infection or inflammation, which may include severe pain, swelling, redness, warmth, limited range of motion, and fever. Common indications include suspected cases of septic arthritis, rheumatoid arthritis, gout, or other inflammatory joint conditions.
- Procedure:
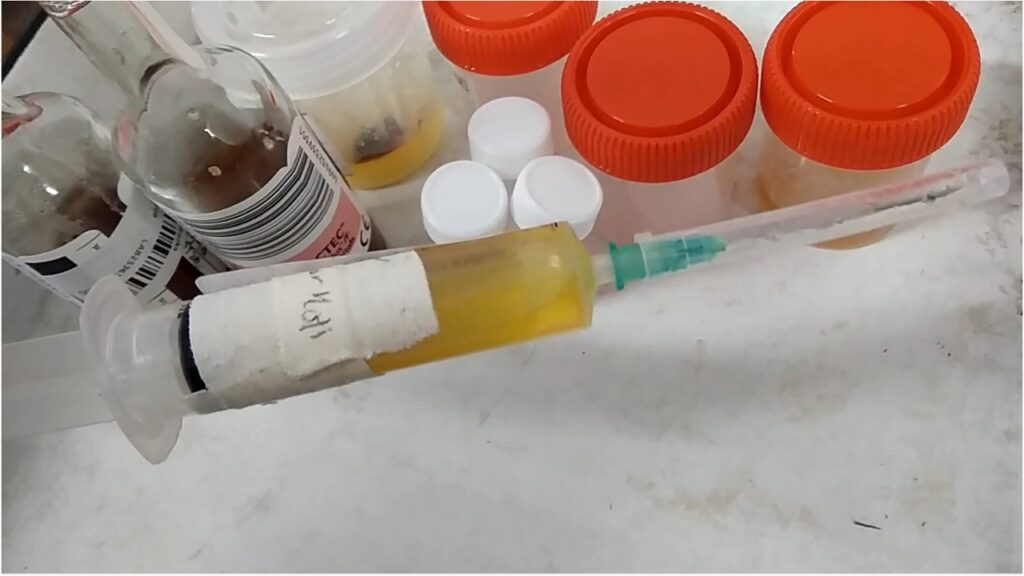
- A trained healthcare professional usually performs the procedure, which involves the insertion of a sterile needle or syringe into the affected joint to aspirate synovial fluid.
- The collected synovial fluid is then sent to a laboratory for analysis.
- In the lab, a portion of the fluid is used to perform a culture, where it is placed on specialized agar plates to encourage the growth of any microorganisms present.
- Another portion of the fluid is used for sensitivity testing, where the isolated microorganisms are exposed to different antibiotics or antimicrobial agents to determine which ones are effective in treating the infection.
- Interpretation:
- Positive culture results indicate the presence of bacteria, fungi, or other pathogens in the joint.
- Sensitivity testing helps identify the most appropriate antibiotics or treatments to combat the specific microorganism(s) responsible for the infection.
- Clinical Significance: Early detection and treatment of joint infections are crucial to prevent joint damage and systemic complications. The results of this test inform healthcare providers about the most suitable antimicrobial therapy, helping improve patient outcomes.
- Limitations: It’s essential to note that synovial fluid culture and sensitivity tests may yield false-negative results if the infection is in its early stages or if the sampling technique is not performed correctly. In such cases, repeat testing may be necessary.
Report
Negative: No growth
Positive: Name of isolated microbe/s and its/their antimicrobial susceptibility testing (AST) result
Clinical Significance
The clinical significance of a Synovial Fluid Culture and Sensitivity Test lies in its ability to provide valuable information for the diagnosis and treatment of joint-related conditions, particularly those involving infections. Here are some key clinical significances of this test:
- Diagnosis of Joint Infections: The test helps confirm or rule out the presence of infections within a joint, such as septic arthritis. Rapid and accurate diagnosis is crucial to initiate appropriate treatment promptly.
- Identification of Causative Microorganisms: By culturing synovial fluid, healthcare providers can identify the specific bacteria, fungi, or other pathogens responsible for the infection. This information is essential for targeted therapy.
- Guidance for Antibiotic Selection: Sensitivity testing determines which antibiotics or antimicrobial agents are effective against the isolated microorganisms. This information allows healthcare providers to prescribe the most appropriate and tailored antibiotic treatment, thereby improving the chances of successful infection resolution.
- Prevention of Joint Damage: Timely diagnosis and treatment of joint infections are critical for preventing long-term joint damage, which can lead to disability if left untreated.
- Reduction of Systemic Complications: Joint infections can lead to systemic complications if not managed properly. The test helps mitigate the risk of complications by identifying and addressing the infection at an early stage.
- Personalized Treatment Plans: The test results allow for the development of personalized treatment plans for each patient, taking into consideration the specific pathogen involved and its susceptibility to antibiotics. This targeted approach can lead to faster recovery and fewer side effects.
- Monitoring Treatment Response: In cases where joint infections are treated empirically before culture results are available, follow-up synovial fluid cultures can be performed to monitor the response to treatment. If the initial treatment is ineffective, adjustments can be made based on the culture and sensitivity results.
- Differentiation of Inflammatory Conditions: Synovial fluid analysis can help differentiate between infectious and non-infectious causes of joint inflammation. This is important because the treatment approaches for these conditions can vary significantly.
- Reduction of Antibiotic Resistance: By tailoring antibiotic therapy to the specific pathogen causing the infection, the test helps minimize the unnecessary use of broad-spectrum antibiotics, which can contribute to the development of antibiotic resistance.
Common Pathogens
The pathogens that are commonly identified through a Synovial Fluid Culture and Sensitivity Test include bacteria, fungi, and, in some cases, viruses. The types of pathogens detected can vary depending on the clinical presentation and risk factors of the patient. Here are some common pathogens that may be found in synovial fluid cultures:
- Bacteria:
- Staphylococcus aureus: This is one of the most common bacteria associated with joint infections, particularly in cases of septic arthritis.
- Streptococcus species: Various Streptococcus species, such as Streptococcus pyogenes and Streptococcus pneumoniae, can cause joint infections.
- Escherichia coli (E. coli): E. coli infections may occur, especially in urinary tract infections that spread to the joints.
- Haemophilus influenzae: This bacterium can cause joint infections, particularly in children.
- Neisseria gonorrhoeae: Responsible for gonococcal arthritis, which often affects young adults.
- Pseudomonas aeruginosa: Commonly found in healthcare-associated joint infections.
- Fungi:
- Candida species: Fungal joint infections, often caused by Candida species, can occur in individuals with immunocompromised conditions or those who have received prolonged antibiotic therapy.
- Mycobacterium tuberculosis: Tuberculous arthritis is a rare but serious form of joint infection caused by Mycobacterium tuberculosis. It may be considered in cases with appropriate risk factors or clinical history.
- Viruses (less common):
- While viral joint infections are less common, some viruses can cause arthritis. Examples include the parvovirus B19 and hepatitis C virus.
It’s important to note that the choice of pathogens to test for in a synovial fluid culture may be influenced by the patient’s clinical history, risk factors, and the suspected source of infection. Additionally, the specific pathogens may vary based on geographic location and local epidemiology.
The Synovial Fluid Culture and Sensitivity Test aims to identify the causative pathogen(s) so that targeted and effective antibiotic or antifungal therapy can be administered. Early identification of the responsible pathogen is crucial for successful treatment and to minimize joint damage and complications.
Keynotes
Here are some key points to remember about the Synovial Fluid Culture and Sensitivity Test:
- Purpose: The test is performed to diagnose joint infections and inflammatory conditions by analyzing the synovial fluid that surrounds and lubricates the joints.
- Indications: It is ordered when a patient presents with symptoms such as joint pain, swelling, redness, warmth, limited range of motion, and fever, which may suggest a joint infection or inflammation.
- Procedure: A healthcare professional uses a sterile needle or syringe to collect synovial fluid from the affected joint. This fluid is then sent to a laboratory for analysis.
- Culturing: In the lab, a portion of the synovial fluid is placed on specialized agar plates to encourage the growth of any microorganisms present, such as bacteria, fungi, or viruses.
- Sensitivity Testing: Another portion of the fluid is used to test the isolated microorganisms for sensitivity to antibiotics or antifungal medications. This helps guide treatment decisions.
- Diagnosis: The test can confirm the presence of joint infections and identify the specific pathogens responsible for the infection.
- Treatment Guidance: The sensitivity testing results help healthcare providers choose the most effective antibiotics or antifungal agents for treating the identified microorganisms.
- Prevention of Complications: Timely diagnosis and treatment are essential to prevent joint damage and systemic complications associated with joint infections.
- Personalized Treatment: The test allows for tailored treatment plans, considering the specific pathogen and its susceptibility to medications.
- Monitoring Response: In some cases, follow-up synovial fluid cultures may be performed to monitor the response to treatment and make adjustments if necessary.
- Limitations: The test may yield false-negative results in the early stages of infection or if the sampling technique is not performed correctly. Repeat testing may be needed in such cases.
- Differentiation: It can help differentiate between infectious and non-infectious causes of joint inflammation, guiding appropriate treatment approaches.
- Reduction of Antibiotic Resistance: Targeted antibiotic therapy based on sensitivity results helps reduce the unnecessary use of broad-spectrum antibiotics, which can contribute to antibiotic resistance.
- Patient Outcomes: The test plays a crucial role in improving patient outcomes by providing the information needed for accurate diagnosis and effective treatment.
Further Readings
- Medical Journals and Research Articles:
- Look for research articles in medical journals such as the Journal of Clinical Microbiology, Clinical Infectious Diseases, and the Journal of Rheumatology. These journals often publish studies related to synovial fluid analysis and joint infections.
- Textbooks:
- “Clinical Microbiology Procedures Handbook” by the American Society for Microbiology (ASM) provides detailed information on microbiological testing techniques, including synovial fluid cultures.
- Medical Websites and Organizations:
- Explore websites of reputable medical organizations like the Centers for Disease Control and Prevention (CDC), the American College of Rheumatology (ACR), and the Infectious Diseases Society of America (IDSA) for guidelines, resources, and research related to joint infections and diagnostic procedures.
- PubMed:
- Utilize the PubMed database to search for specific research papers, reviews, and clinical guidelines related to synovial fluid culture and sensitivity testing. PubMed is a valuable resource for accessing a wide range of medical literature.
- Textbooks on Rheumatology:
- Textbooks on rheumatology, such as “Rheumatology: Diagnosis and Therapeutics” by John Klippel and John H. Stone, often contain sections on the diagnosis and management of joint-related conditions, including septic arthritis.
- Clinical Practice Guidelines:
- Check for clinical practice guidelines issued by medical organizations like the IDSA or ACR. These guidelines often include recommendations on the diagnosis and management of joint infections.
- Online Medical Courses and Webinars:
- Consider enrolling in online courses or attending webinars related to infectious diseases, microbiology, or rheumatology, which may cover topics related to synovial fluid analysis.
- Medical Databases:
- Explore medical databases like UpToDate and DynaMed for comprehensive, evidence-based summaries and guidance on synovial fluid analysis and related diagnostic tests.
- Medical Conferences:
- Keep an eye out for conferences and symposia in the fields of infectious diseases, rheumatology, and microbiology, where experts often present the latest research findings and updates on diagnostic procedures.
- Consultation with Healthcare Professionals:
- If you have specific questions or require in-depth information, consider consulting with healthcare professionals, such as rheumatologists, infectious disease specialists, or clinical microbiologists, who can provide expert insights and recommendations.